Unlocking the Mystery of Autism: Can a Cold or Flu During Pregnancy Play a Role?

For decades, scientists have been trying to figure out why some children develop autism. While we know that genes are a big part of the puzzle, recent research is shedding light on how something as common as a cold or the flu during pregnancy could also contribute. A new study from the Cold Spring Harbor Laboratory (CSHL) in New York suggests that when a mother’s immune system fights off a virus, it may unintentionally affect the developing brain of her baby—especially if that baby is a boy.

How Could a Cold or Flu Affect the Baby?
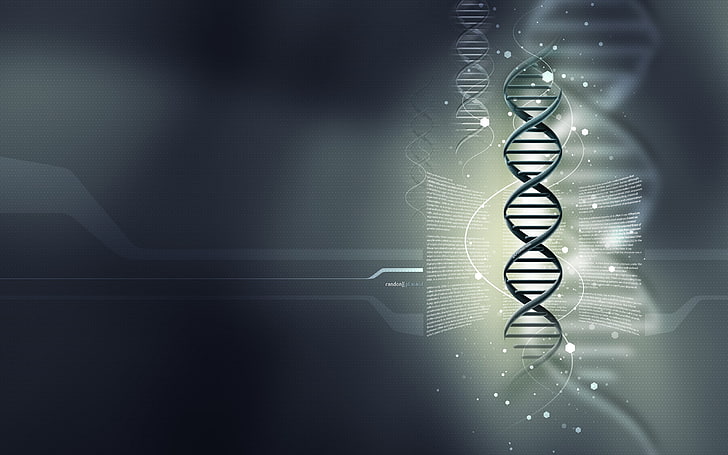
When a pregnant woman catches a cold or flu, her immune system goes into overdrive to protect her body. This immune response, known as maternal immune activation (MIA), releases small immune cells called cytokines and chemokines. These cells help fight off infections, but they can also cross the placenta—the barrier that separates the mother’s blood from the baby’s. Once these cells reach the baby, they can enter the developing brain and potentially cause disruptions.
This is especially concerning because a fetus’ brain is highly sensitive to what’s happening in the womb. Any disturbance, like a surge in immune activity, can potentially affect how brain cells connect and communicate. Researchers believe this disruption could be a reason why some children develop autism spectrum disorder (ASD), a condition that affects social skills, communication, and behavior.

Why Are Boys More Affected?
One striking discovery from the CSHL study is that male embryos seem to be more vulnerable to these immune changes than female embryos. In their study with mice, about one-third of male embryos exposed to a simulated viral infection showed signs of slowed brain development that could be linked to autism. Interestingly, female embryos seemed to be mostly protected from these effects.
This finding aligns with what we already know—autism is more common in boys than girls. In the U.S., about four in 100 boys are diagnosed with autism, compared to one in 100 girls. This difference in vulnerability during pregnancy might help explain why.

The Role of the Immune System
The immune system’s response to a virus is powerful and necessary to fight off infections. Cytokines—the small immune cells released during an infection—help protect the body by causing symptoms like fever and body aches. However, in a pregnant woman, these same immune cells could accidentally interfere with the baby’s brain development.
In fact, previous studies have linked MIA with changes in how brain cells (neurons) and their connections (synapses) are organized. If these connections are disrupted, it could reduce the number of neurons and synapses in the baby’s brain—something that’s been associated with autism.

What About Vaccines?
It’s important to note that vaccines, such as the flu shot, don’t have the same effect as a viral infection. Vaccines work by preparing the immune system to fight off a virus without causing the full-blown inflammation that an actual illness would trigger. In fact, vaccines help protect both the mother and baby by passing protective antibodies from mother to fetus, reducing the risk of serious infections.
Santhosh Girirajan, a neurodevelopmental disorder expert at Pennsylvania State University, stresses that vaccines do not cause autism, a fact backed by years of research.
What’s Next for This Research?
Irene Sanchez Martin, the lead scientist on the study, cautions that her research is still in its early stages. Her experiments focused on what happens to a fetus just 24 hours after the mother’s immune system reacts to a virus. There’s still much more to learn about how exactly these immune responses during pregnancy may lead to autism, and her research didn’t explore other factors that could also affect the immune system, like obesity or underlying conditions.
Still, this research provides a new clue in understanding autism’s complex causes. More than 5.4 million people in the U.S. are diagnosed with autism, and while up to 80% of cases are thought to be genetic, this leaves a significant portion of cases influenced by other factors, like environmental conditions in the womb.
Sanchez Martin and other scientists are hopeful that by continuing to study how prenatal inflammation affects brain development, they might one day be able to predict autism risk earlier—perhaps even before a child is born. Early diagnosis is key since it helps families access therapies and support sooner.
Autism on the Rise
Autism diagnoses are increasing across the U.S. The Centers for Disease Control and Prevention (CDC) reported that in 2000, about one in 150 eight-year-olds had autism. By 2020, that number had jumped to one in 36. This rise is partly due to better awareness and improved screening by doctors, but it also suggests we still have a lot to learn about the causes of autism.
While there’s no single answer yet, studies like the one from CSHL are bringing us closer to understanding how the environment in the womb, including something as simple as a cold or flu, may play a role in shaping a baby’s brain. This research gives hope that one day we’ll be able to intervene earlier, offering families more support and better outcomes for children with autism.
![100+] Pregnant Woman Wallpapers | Wallpapers.com](https://wallpapers.com/images/hd/pregnant-woman-baby-bump-sitting-down-uwu8ykihqmctbd5c.jpg)
In Conclusion
Autism is a complex condition with many possible causes, but thanks to groundbreaking research, we’re beginning to unravel one of its many mysteries. While genes play a huge role, the immune system’s response to something as common as a cold or flu during pregnancy could also be a key factor. With continued research, scientists hope to better understand how we can protect developing brains and support early intervention for autism.